Intraoperative Cell Salvage (10-15 min read)
This week we’ll be talking all about cell salvage! It’s becoming an increasingly popular topic in the FRCA OSCE examination and with its growing evidence base and popularity, I thought it would be helpful to learn about.
I’ve written this blog post in an “Examination style” of Q&A, to give you a flavour of the types of questions that can come up in relation to cell salvage, both in the Primary and the Final FRCA examinations. I have also broken down my answers into short bullet points where I think the marks are likely to lie with certain “buzz words” highlighted/underlined.
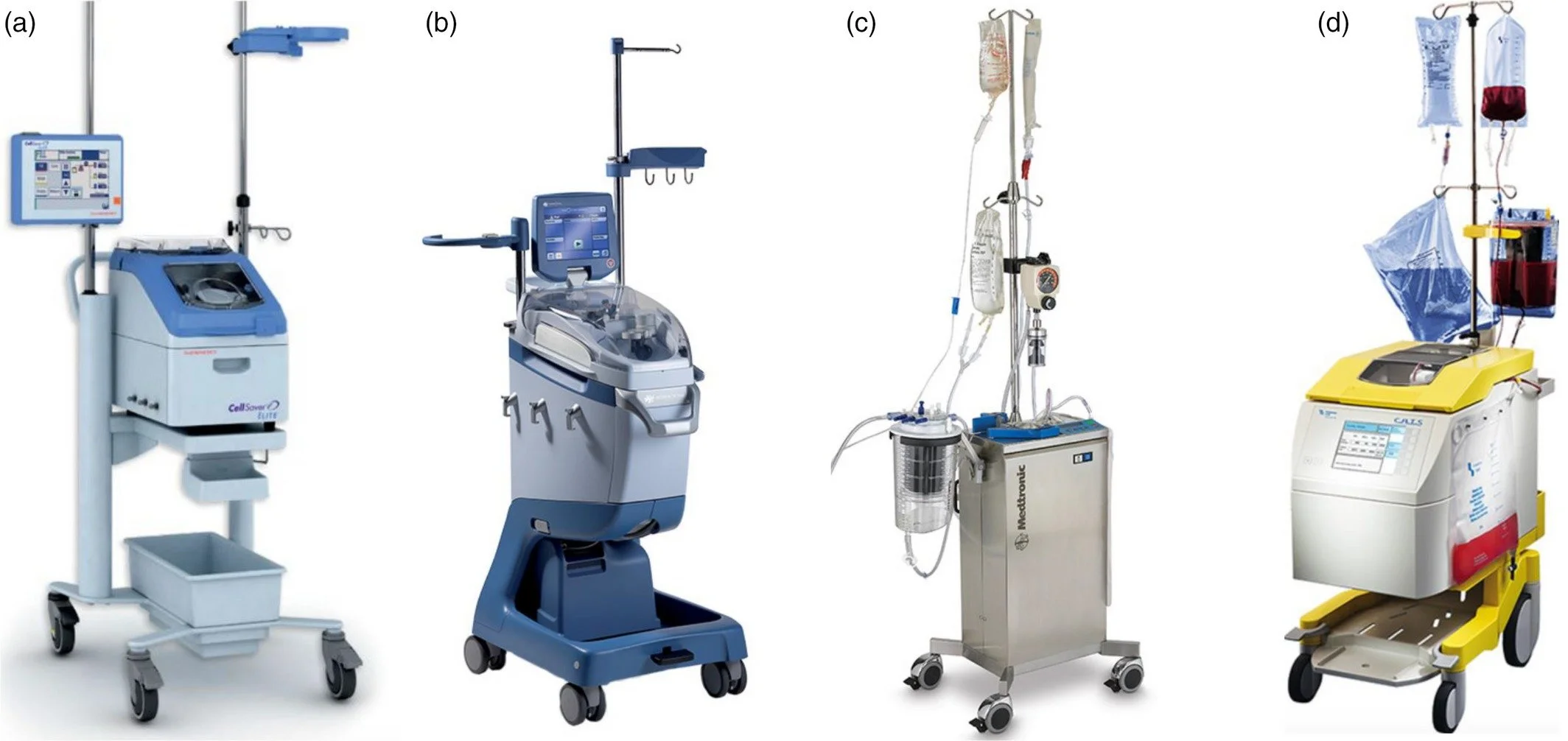
Recognise any of these Cell Salvage machines? Get to know yours next time you’re at work!
The Basics
What is intraoperative cell salvage? (ICS)
It is a method of autologous red cell transfusion by :
1. Harvesting red cells shed during surgery,
2. Processing and preparing them for safe return to the patients’ own circulation
3. Either during or (immediately) after surgery
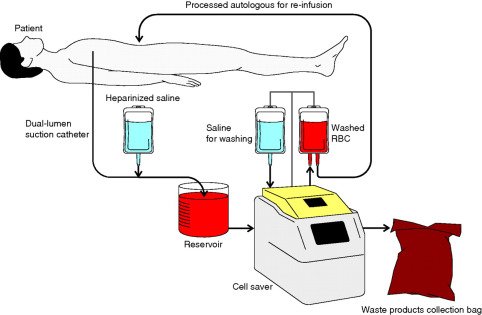
What are the main principles/steps of ICS?
Automated or semiautomated process
1. Collection/Suction – blood is collected by aspiration directly from the surgical site or by washing bloody surgical swabs*
Blood is then combined with an anticoagulant (heparin or citrate)
2. Filtration – usually 150micron
3. Separation by centrifugation – isolated from other constitutes according to their density and mass
4. Disposal – waste products discarded
5. Wash & resuspension– in saline 0.9%
6. Reinfusion – presented as a high haematocrit (HCT) (approx. 60%) suspension of packed red cells in normal saline
*swab washings are used when there is expected to be a large amount of blood collected. How? Bloody swabs are soaked and gently squeezed to minimise red cell trauma in normal saline 0.9% and combined with unfractionated heparin (UFH).
Saline should be licensed for IV infusion, NOT irrigation.
The vessel in which they are soaked should be positioned within the clean air area to minimise airborne contamination.
Many ICS machines offer “Emergency protocols” – they increase production of red cells at the expense of greater red cell loss (higher spin rates and reduced wash cycles) – takes a few minutes when time critical
Cell salvage schematic diagram
The Details:
By what means can blood be collected for ICS?
1. Aspirated directly from the surgical site
2. Washing blood surgical swabs
What micron filter is usually used in a ICS machine?
· 150 micron (40-150)
What are the waste products of centrifugation?
· Free Hb
· Anticoagulant
· Plasma proteins
· Clotting factors
· White blood cells
· Platelets
· Squames
· Bone fragment
· Bacteria
· Fat
What are the different methods of separation by centrifugation?
Automated or semiautomated process
1. Fixed bowl system
· Conical rotating bowl
· Centrifugal force separates the blood – more dense cellular fragments collected at the bottom
· Red cells retained
· Layer above (supernatant) is removed via the waste port
· Machine detects when an adequate volume of red cells has been collected and initiates washing
· When washing is not automatically triggered – it can be programmed to wash a ‘partial bowl’ but this requires an increased wash volume to ensure adequate contaminant removal.
2. Variable volume disk system
· Similar to above but silicone diaphragm allows washing at variable volumes (as opposed to fixed as above) with a fixed HCT.
· Advantages – can be used when blood collection is slow and volume is low; allows for several small batches before washing
3. Continuous rotary system
· Removal of supernatant, concentration and washing of red cells is continuous
· Advantages - can be done with small volumes of blood loss
How can red cells be damaged during the collection —> reinfusion process?
· Before aspiration if exposed to:
o Hypotonic solutions e.g water
o Agents that damage the cell membrane – urine
o Substances that promote coagulation
o Mechanical trauma – from aspiration/narrow bore suction catheters
How can red cell damage be prevented?
· Bespoke ICS suction systems that automatically alter the suction pressure to reduce damage and optimise aspiration
· Suctioning from pooled red cells as opposed to skimming over shallow collections of blood
What anticoagulant solution is added to blood during the blood collection?
· Heparin
· Citrate (citrate dextrose solution-A)
Reinfusion process:
· Should take place within 6 hrs
· Trained and monitored environment
· Blood to be reinfused – clearly labelled
· Flush IV line and administer blood through a blood giving set
What specific cautions are taken prior to and whilst administering cell salvaged blood?
· Do not give under pressure
· Flush IV line prior to administration - certain drugs e.g. IV paracetamol can cause the red cells to clump
Advantages and Disadvantages:
When might using cell salvage prove useful intraoperatively?/be considered?
When significant blood loss is expected e.g cardiothoracic/vascular surgery
When finding donor blood may be difficult for patients who have rare blood groups/antibodies
What are the potential benefits of ICS blood?
1. Higher concentrations of 2,3 DPG and ATP
2. Tissue oxygen delivery superior
3. Salvaged red cells retain their elliptical profiles and deformability better
o Evidence supports early reinfusion, as oxygen carriage and deformability degrade over time – reduction in function most significant >=6 hours after collection
4. Reduction in need for donor blood and issues that come with it, particularly immunomodulatory effects, transfusion reactions (ABO mismatch), transfusion complications (infection transmission)
5. Salvaged red cells do not initiate negative immunomodulatory effect when infused in perioperative period
o Immunomodulation only seen when stored autologous red cells are reinfused, supporting further the need to re-infuse as quickly as possible
o Dose dependent transfusion related immunosuppression (TRIM) with allogenic blood àincreased risk of developing post op infection, possible increased risk of tumour or metastatic growth
6. No restrictive transfusion triggers
7. Volume expansion – viscous
8. May be morally satisfactory option for cultural groups who would object to donor blood transfusion
9. Reduced post op morbidity from reduced o2 delivery/immunosuppression related infection
o Reduces post-operative anaemia
o Reduces dose of allogenic transfusion
o à earlier mobilisation, decreased LOS, reduces ward staff workload
10. Economic benefit – can reduce demand on precious blood bank stocks
Note: concentration of free Hb in ICS is small and is likely to be less than that seen in allogenic transfusion
What are the risks of allogenic blood transfusion that you won’t see with autologous blood transfusion?
Risk of acute transfusion reaction by:
· Antigen sensitisation
o Concentrations of antibodies may reduce over time, and may only sensitise on re-exposure àdelayed haemolytic reaction
o E.g. Kell antigen – following exposure in childbearing female à increased risk of haemolytic disease of the fetus and newborn (HDFN)
Name some antigens which may be sensitised following a transfusion (that aren’t routinely screened for) from donor blood samples:
1. Kelly
2. Duffy
3. Lutheran
What are the risks involved with ICS?
1. Bacterial contamination
2. Emboli (fat, amniotic fluid)
3. Transfusing unwanted substances e.g cancer seeding, non-sterile procedures – bacterial spread e.g. bowel perforation
a. there is some suggestion that using leucocyte depletion filters / a second suction system to remove undesirable substances before using the cell salvage suction may help.
What are the potential disadvantages of ICS?
1. Correct patient selection is important
2. Trained and committed staff required – labour intensive, increased diligence req.
3. Financial investment – training, machinery, disposables
4. Reinfusion hypotension – unclear as to why this occurs – bradykinin release and acute hypocalcaemia has been proposed
a. Remember to rule out other causes of intraop hypotension
5. In emergencies – red cells may not be immediately available and may req. use of allogenic red cells to temporise and hypovolaemic issues.
6. Salvaged blood contains clinically insignificant concentrations of clotting factors, platelets – when large volumes are processed, the use of clotting factors, platelets and calcium may be necessary.
7. Citrate contained in the blood can cause system coagulopathy/caution required in liver dysfunction. Calcium may need to be administered to neutralise the citrate.
Complications:
How would you manage a suspected case of reinfusion hypotension intraop?
Simultaneously investigate, assess and manage the patient
1. Stop infusion
2. ABCDE approach, 100% oxygen
3. Look for other potential causes - ?hypovolaemic ?haemorrhagic
4. Treat with vasopressors if required
5. If all other causes excluded, and blood still deemed to be required then re-start infusion at slower rate
Special considerations:
When might leucocyte depletion filters (LDFs) be used?
· Commonly used in cancer surgery
· Concern over heavy bacterial contamination
LDF’s:
· Require priming
· Significantly REDUCE rate of reinfusion
· Reinfused hypotension = well recognised complication
o Squeezing the LDF (attempting to force the flow of red cells through it under pressure may accentuate this problem)
What is the filter size of a standard blood giving set?
· 200 microns
Summary:
Now you’re a Intraoperative Cell Salvage Champion! In this post you have learnt about what cell salvage is, the different stages involved, its uses, advantages/disadvantages as well as risks/complications and special considerations!
Comment below if you’d like to see us write about a particular topic!
References:
Intraoperative cell salvage - C. Carroll, F. Young, BJA Education, 21(3): 95e101 (2021), doi: 10.1016/j.bjae.2020.11.007
Equipment in Anaesthesia, Daniel Aston
Cell salvage images - https://onlinelibrary.wiley.com/doi/full/10.1111/vox.12527 (last accessed 5.1.22)
Cell salvage diagram - https://www.bjanaesthesia.org.uk/article/S0007-0912(17)33465-7/fulltext - (last accessed 5.1.22)